Most of us are familiar with the story of the little boy who cried wolf. In case you aren’t aware of the premise and lesson of this fable, let me give you a little backstory.
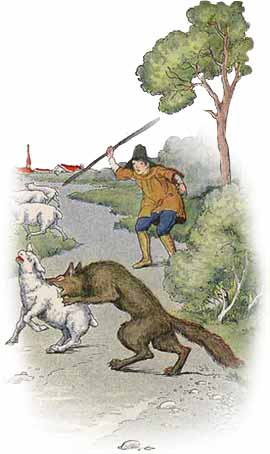
The fable basically concerns a boy, a shepherd, who likes to play practical jokes on his neighbors and people in his town. He constantly goes running down from the pasture lands screaming that the town’s sheep are being attacked by wolves. There’s no wolf, and the town’s people get sick of his pranks and stop believing him. But then, a wolf really does show up and ends up eating all the sheep because no one believes the kid’s cries for help. Moral of the story: this shows how liars are rewarded: when you really are in need and tell the truth, no one will believe you.[1]
Since the release of the proposed changes to the 21st Century Cures Act earlier in 2019, little “criers” have been coming out of the pastures scream about wolves of all shapes and varieties. They have hired lobbyists, created special interest groups, use every political channel possible (even some with questionable moral/ethical concerns), and started an uproar that would concern even the hardiest characters of fairy tales and the most harden heroes of comic books.
The little shepherd has a new face. Well, to be honest, he has a number of new faces. But I think the face that sticks out most has the initials E.H.R.
Back in June, the Electronic Health Records Association, a division of HIMSS, had what they called two “Congressional briefings” – one for members of the House and another for members of the Senate, intended to “…share with policymakers the Association’s perspective…” on the changes to the 21st Century Cures Act.[2] Let’s not use words to mask what this “briefing” really was: it was lobbying done outside the bounds of Congress and thus outside the bounds of public disclosure to influence lawmakers to see things the way that this organization sees them. Call a snake what it is – a snake.
So, the EHRA wanted Congress to know that they were extremely concerned about the proposed changes, and they explained why to a certain degree. However, if you dig a little deeper, it’s easy to see why they are so worried, and why they felt it so necessary to cry “WOLF’ so loudly that they needed to invite Congress to attend a meeting. Let’s shave away all the fluff and get down to the real reason EHRs have a problem with these changes. It’s profit, plain and simple.
If you read the event summary, right out of the starting gate, the EHRA states they are concerned about “…the proposed price controls and licensing of intellectual property that will override market forces and inhibit innovation.”[3] In reading this, I thought they might be a little less obvious in their real intentions, but they went for broke upfront.
The event summary states “…the proposed requirement to limit companies’ ability to charge fees beyond the cost of recovery devalues the work of software developers and penalizes innovation and efficiency by overriding market forces and profit-driven motivations for investments in new technology.”[4] By companies, they mean EHRs. This is a situation that EHRs created themselves and now they have to own it.
The proposed changes to the 21st Century Cures Act to strip away an EHRs ability to charge a fortune for their software, integrations, and add-ons for healthcare systems and others engaged in healthcare. The changes make it very clear that health IT developers cannot prohibit or restrict the communication of data under new guidelines for information blocking.[5] While parts of the overall definition are broad and vague, there is little doubt cast in the direction of EHRs. Information blocking by health IT is that which “…is likely to interfere with, prevent, or materially discourage access, exchange, or use of electronic health information.”[6]
EHR companies know that the implementation of these changes will impact their ability to monetize integration. Their loss will occur in two forms: the outrageous prices they charge for their systems and the money-in-the-bank integration barriers they have been milking since EHRs were incentivized in the HITECH Act.
Healthcare systems need to be able to afford EHRs if they actually want to be able to provide the best care. Furthermore, those people who interact with healthcare data need to know that they have the best and most correct information possible. The changes proposed by the ONC are the next step towards making sure clinicians have the data they need to make good decisions for patients.
A recent news article stated that the cost of EHR implementations in 2017 ranged anywhere from $25 million to $10 billion.[7] This same article states that four hospitals each netted losses well over $20 million dollars in the months following their EHR rollouts, as well as huge percentage losses in productivity.[8] Given these exorbitant costs and losses, it would be impossible to imagine that in rural and urban areas where this technology is needed the most they can scarce afford it. Living in Tennessee, we learn the sad news on a weekly basis of yet another rural healthcare system that is forced to close due to budgeting issues. They could never sustain a loss on this scale – financially or in productivity. One has to wonder if Judy Faulkner, Epic Systems CEO, gave any thought to the suffering of rural and urban healthcare systems that cannot afford Epic products when she stated in a recent article that she tells her employees to “have fun, do good, and make money.”[9]
I doubt many medical professionals and practitioners are having a lot of fun given the prevalence of data that shows a plethora of negatives in dealing with EHRs on the whole. Since 2010, EHR-related medical malpractice claims and tripled, with a total of 216 cases closed.[10] In most of those cases, the lawsuit stemmed from a failure within the software or an issue with data interoperability.
A recent survey of physicians found that they had little love for EHRs, citing that the programs don’t do what they are needed to do, that they fail to interact with other systems, that they are not user-friendly, and that the data is redundant, missing, or inaccurate.[11] Yet another survey of physicians stated that 60% of them felt that EHRs has a negative impact in the exam room, taking away time from their patients. Those same physicians said if they had it to over again, they would not go with the same EHR company, but also stated that they would not be willing to change due to the hassles of getting the system up and running in the first place.[12] It’s no wonder that the American Hospital Association has been a strong voice against the rollout of the ONC’s proposed changes, as they see the new guidelines as crippling for the progress of interoperability.[13] No doubt most hospitals remember how hard it was to even come online initially with the EHR. I would be terrified of the slightest change, too, if I had to live with that memory.
The other end of the cash cow (or sheep) deals with interoperability and one of the things we do at Interoptex: Healthcare IT Integration. The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 was an ambitious policy effort to increase the adoption of electronic health records (EHRs).[14] It was prompted by evidence that the use of EHRs can substantially improve the quality and efficiency of care delivered. While the HITECH Act propelled the move from paper to digital records, it did not address or create an infrastructure for data interoperability. Healthcare information systems and EHRs have to be interoperable in order to provide the best care to the patient, as not one healthcare system or doctor within a single system will fit every patient’s needs.
As a result of this lack of interoperability, EHRs have made a small fortune by erecting barriers to sharing information and charging outrageous prices for integrations.[15] Using intellectual property copyrights as their legal soapbox and defense, they have prevented smaller organizations and those without the financial ability from access to needed information about patients. If you can’t pay the fees, you are blocked from the information you need and the efficiency to operate that you not only desire but need to provide the best care possible. But remember: have fun, do good, make money.
One great example of how high EHRs have created barriers around themselves is the continued use of FAX machines in healthcare. A recent op-ed in the Wall Street Journal argued that, while we live in an age where artificial intelligence can diagnose lung cancer more accurately than humans, a vast majority of healthcare systems still rely on FAX machines due to siloed information because of a lack of interoperability and information blocking.[16] Critics of the proposed changes posit, paradoxically, that the ONC’s changes will hinder technological growth, while their own EHRs have created an environment that is still dependent on 40-year-old technology to send and receive data that has to be manually entered. So, which is it? Who created this problem to start with? Should we blame it on the FAX machine?
Technology innovators, like Interoptex, created ladders over their barriers in the form of integration teams. We found ways using every preposition we could think of to get to the root of the problem. We’ve continued to build products despite and in spite of the challenges created by siloed health information.
Not surprising, however, one EHR company wanted to double up on the interoperability profits and created their own integration company to scale the barrier walls they created and make even more money. How’s that for crying wolf out both sides of your mouth?
So, what does all of this really mean? It means the wolf-criers are like the shepherd. There is no wolf, but some bad actors would love for you to think so. While there are some changes and processes that will need to be addressed in the 21st Century Cures Act, the arguments that were made in those June briefings were intended to strike fear into practitioners, providers, and anyone who would listen. The problems that exist today are the direct result of greed on the part of proprietary software companies that fear losing the steady stream of cash made from information blocking. It’s not an issue of intellectual property, or even the EHR system itself. It’s a fear of lost profit, plain and simple.
[1] Aesop. The Shepherd Boy and the Wolf. http://read.gov/aesop/043.html
[2] Event Summary - 21st Century Cures Act: Interoperability, Information Blocking, and the Impacts on Healthcare. (June 25-26, 2019) HIMSS Electronic Health Record Association. https://www.ehra.org/sites/ehra.org/files/EHRA%20Congressional%20Briefing%20Summary%20-%20Interoperability%20Information%20Blocking%20and%20the%20Impacts%20on%20Healthcare.pdf
[3] Ibid, pg.1: para. 2.
[4] Ibid, pg. 2: para. 1.
[5] Anthony, E.S. & Lipinski, M. (Feb 2019). 21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program Proposed Rule. Slide 16. https://www.healthit.gov/sites/default/files/page/2019-02/HITACNPRMPresentation.pdf
[6] Ibid, slide 29.
[7] Dyrda, L. (19 Sep 2019). Three Times EHR Adoption Led to the Hospital, Health System Operating Loss in the Past Year. Becker’s Health IT & CIO Report. https://www.beckershospitalreview.com/ehrs/3-times-ehr-adoption-led-to-hospital-health-system-operating-loss-in-the-past-year.html
[8] Ibid.
[9] Drees, J. (16 Sep 2019). Epic CEO Judy Faulkner on ‘Yes, if’ Strategy Behind Company’s Culture, Success. Becker’s Health IT & CIO Report. https://www.beckershospitalreview.com/ehrs/epic-ceo-judy-faulkner-on-yes-if-strategy-behind-company-s-culture-success.html
[10] Drees, J. (28 Aug 2019). EHR-Related Medical Malpractice Claims Tripled Since 2010, Study Finds. Becker’s Health IT and CIO Report. https://www.beckershospitalreview.com/ehrs/ehr-related-medical-malpractice-claims-tripled-since-2010-study-finds.html
[11] Garrity, M. (27 Aug 2019). Five Biggest Problems Physicians Have with Their EHRs. Becker’s Health IT & CIO Report. https://www.beckershospitalreview.com/ehrs/5-biggest-problems-physicians-have-with-their-ehrs.html
[12] Park, A. (23 Oct 2019). 60% of Physicians Say EHRs are Harming Patient Engagement. Becker’s Health IT and CIO Report. https://www.beckershospitalreview.com/ehrs/60-of-physicians-say-ehrs-are-harming-patient-engagement.html
[13] Pifer, R. (26 June 2019). Industry Interoperability Concerns Plague TEFCA Draft. Healthcare Dive. https://www.healthcaredive.com/news/industry-interoperability-concerns-plague-tefca-draft/557208/
[14] Blumenthal D . Stimulating the adoption of health information technology . N Engl J Med . 2009 ; 360 ( 15 ): 1477-9
[15] Physicians Clinical Registry Coalition’s Letter to the ONC 21st Century Cures Act Certification Program – Documentation of the Fees and Charges Related to Integration.
[16] Minor, L. (19 Sep 2019). Why Your Doctor’s Office Still Depends on a FAX Machine. Wall Street Journal. https://blogs.wsj.com/experts/2019/09/19/why-your-doctors-office-still-depends-on-a-fax-machine/
← Back to portfolio